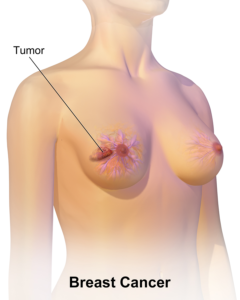
Image : “Breast cancer reflection” by williami5. License:
CC BY 2.0
Overview of the ASCO Guidelines
- Detection of breast cancer recurrence
- Induction of second primary cancers by chemotherapy and radiotherapy
- Cosmetic blemish from a mastectomy
- Physical and psychosocial long-term effects of breast cancer and its treatment
- General health promotion, care coordination, and practice implications
Identification of these effects is guided by the American society of clinical oncology (ASCO) where a guideline is formulated after a comprehensive literature search is conducted by a panel of experts. The level of evidence for each recommendation in a guideline usually follows the following scheme (see Table 1).
| Level of Evidence | Criteria |
| I | Meta-analyses of randomized control trials directly related to the subject “breast cancer survivors in this scenario”. |
| IA | Based on the results of a single randomized control trial of subjects belonging to the targeted population of the guideline “breast cancer survivors”. |
| IB | Based on the results of randomized control trials of a less specific, but still related population “cancer survivors in general for instance”, |
| IC | Based on the results of a randomized control trial related to similar outcome measures in a non-related study population. |
| IIA | Based on the results of non-randomized control trials on the same targeted population “breast cancer survivors”. |
| IIB | Based on the results of a non-randomized control trial on a related population “cancer survivors in general”. |
| IIC | Based on the results of a non-randomized control trial related to similar outcome measures in a non-related study population. |
| III | Case-control and prospective cohort studies targeting the same population “breast cancer survivors”. |
| 0 | Expert opinion or retrospective/cross-sectional studies. |
| 2A | Based on the National Comprehensive Cancer Network Clinical Practice Guidelines in Oncology. |
Surveillance for Breast Cancer Recurrence
After treating primary cancer, the patient is usually followed by a primary health care provider. One of the most important goals of this follow-up is the early detection of any local recurrence via surveillance. This can be achieved with a proper history and physical examination, screening of the previously treated breast for a local recurrence, and the untreated breast for a new primary breast cancer, performing routine laboratory tests and imaging studies if needed, and making sure that the patient is adhering to endocrine treatment.
The following summarizes the recommendations by an ASCO panel related to the surveillance for breast cancer recurrence:
History and Physical (Level of Evidence 2A)
- Individualize follow-up care to the patient’s age, specific diagnosis, and treatment protocol as set by the expert oncologist
- Detailed cancer-related history and physical examination every 3 to 6 months for the first 3 years after the treatment of primary cancer
- Detailed cancer-related history and physical examination every 6 to 12 months for the next two years
- Detailed cancer-related history and physical examination annually thereafter
Screening the breast for local recurrence and the other side for a new primary cancer (Level of Evidence 2A):
- If the patient underwent a unilateral mastectomy, she should be referred for an annual mammography of the untreated breast
- If the patient underwent a lumpectomy, she should receive an annual mammography of both breasts
- Do not refer for routine MRI screening unless the patient is considered as high-risk for breast cancer recurrence
Laboratory tests and Imaging (Level of Evidence 2A)
- Do not perform any routine laboratory testing
- Do not perform any other imaging studies, except for mammography
- Limit MRI to high-risk patients only
Signs of Recurrence (Level of Evidence 2A)
- Patients should be educated about the signs and symptoms of a recurrence
- Patients should be instructed and educated about how to perform a self-examination of the breasts
Risk Evaluation and Genetic Testing (Level of Evidence 2A)
- The first and most important clue towards a possible genetic predisposition is obtained from family history
- Genetic counseling is needed if a strong family history of breast, colon or endometrial cancer; or age younger than 60 years with a triple-negative breast cancer
Endocrine Treatment Adherence (Level of Evidence 2A)
- Patients should be counseled about the importance of adherence to antiestrogen therapy.
- Symptomatic treatment of the side-effects of antiestrogen therapy improves adherence.
Screening for Second Primary Cancers
Patients with a previous history of cancer are at an increased risk of developing a second primary cancer for several reasons, including genetic predisposition, the use of chemotherapy, and the use of radiotherapy. The main cancers that are more commonly reported in breast cancer survivals are cervix carcinoma, colorectal cancers, endometrial cancers and lung malignancies. The following table summarizes the current recommendations as per the ASCO guidelines for screening for second primary cancers.
| Cancer Site | Targeted Population | Screening Test | Recommendations |
| Colorectal | Age: 50 years | Fecal occult blood testing | Annual testing should be started at the age of 50 years.
Colonoscopy should be performed every 10 years starting at age 50. |
| Cervix | Age 21 to 65 years | Pap smear and human papillomavirus DNA testing | Aged 21 to 29 years:
Aged 30 to 65 years:
- HPV DNA test and Pap smear every 5 years.
Aged 65 years:
- If 3 consecutive Pap smears are negative, STOP screening.
- If 2 consecutive HPV DNA tests are negative, also STOP screening.
|
| Endometrial | At menopause | | At the time of menopause, women should be instructed to report any episode of bleeding from now on. |
| Lung | Current or previous history of smoking.
Aged 55 to 74 years.
30 pack-y-history. | Low-dose helical computed tomography scan of the lungs | |
Assessment and Management of the Adverse Effects of Breast Cancer and its Treatment
The long-term adverse effects of breast cancer treatment are dependent on the type of treatment, duration of treatment, the use of chemotherapy, the use of hormone treatment and the age of the patient. Treatment of breast cancer can include surgery, radiation therapy, chemotherapy, biologically targeted therapy, and endocrine antiestrogen therapy. The following table summarizes the current ASCO recommendations for the management of the adverse effects of breast cancer treatment in breast cancer survivors.
| Category | Recommendation | Level |
| Body image concerns |
- Assess the patient’s concerns about their body appearance, especially after a mastectomy.
- Discuss available breast reconstructive options.
- Refer to psychosocial care if needed.
| 0
0IA |
| Lymphedema |
- Encourage the patient to lose weight.
- Refer to a specialist if lymphedema develops.
| 0
0
|
| Cardiotoxicity |
- Monitor lipid levels and blood pressure.
- Educate the patient about the symptoms of heart disease, and encourage them to follow a healthy lifestyle.
| 0
I
|
| Cognitive impairment |
- Encourage the patient to talk about cognitive changes and deficits.
- Refer to specialist care if cognitive impairment is suspected or confirmed.
| 0
IA |
| Anxiety and depression |
- Assess the patient for signs and symptoms suggestive of anxiety or depression.
- Stratify patients according to age, socioeconomic status, and social support into low risk and high risk for depression.
- Provide in-office counseling and pharmacotherapy if needed.
| I
IIII |
| Fatigue |
- Look for and treat any organic cause, such as anemia or thyroid dysfunction.
- Do not attribute fatigue to mood disorders before performing an adequate check-up.
| 0
I |
| Bone health |
- Refer post-menopausal women for a baseline DEXA scan.
- Repeat DEXA scan every 2 years for women taking an aromatase inhibitor.
- Repeat DEXA scan every 2 years for premenopausal women taking tamoxifen or GnRH agonist, and for women who develop premature menopause.
| 0
0
0
|
| Musculoskeletal health |
- Inquire about the presence of pain.
- Refer to physiotherapy and/or alternative medicine approaches.
| 0
III
|
| Pain |
- Assess the characteristics of pain if present.
- Provide pharmacotherapy for pain if needed.
- Refer to a specialist if the etiology of pain is determined.
- Assess the possibility of peripheral neuropathy.
- Offer duloxetine for patients with neuropathic pain.
| 0
I
0
0
IB
|
| Infertility |
- Refer women of childbearing age who become infertile after treatment to an assisted reproductive specialist.
| 0 |
| Sexual health |
- Inquire about symptoms that could affect sexual intimacy.
- Treat possible causes of sexual dysfunction.
- Offer non-hormonal vaginal lubricants for vaginal dryness.
- Refer to psychosocial and sexual counseling therapy.
| 0
0
IA
IA
|
| Premature ovarian failure |
- Treat symptoms with selective serotonin reuptake inhibitors, gabapentin, and lifestyle modifications/
| IA |
Other ASCO Recommendations Related to Breast Cancer Survivors
Primary health care providers should provide patients with information about their specific diagnosis, its treatment, and the potential adverse effects of such a treatment (level of evidence 0). Vigorous aerobic exercise and strength training exercises are recommended in all patients, including those who receive chemotherapy for breast cancer (level of evidence IA).
The patients should be encouraged to follow a healthy lifestyle, eat more vegetables, and avoid saturated fats (level of evidence IA). Patients with a previous history of breast cancer, like all other patients and healthy subjects, should be encouraged to stop smoking if they are smokers (level of evidence I).
The primary care physician should keep in contact with the oncology team. It is also recommended to include the patient’s family in the decision-making process whenever needed (level of evidence 0).

Comments
Post a Comment